Direct Access and Dental Therapy in 2023
Taking a deep dive into what it means to utilise a Direct Access Dental Therapist in general practice. The tide is turning and Dental Therapy is more popular now than ever. What can a Dental Therapist add to your practice and how does it work?
In 2023 more dental practices than ever are turning to dental therapists to support their service provision. Dental therapists are becoming more vocal about utilising their full skill set and dental teams are beginning to appreciate the opportunities that working with dental therapists can present.
Working under Direct Access means that a Dental Therapist or Dental Hygienist is seeing and treating a patient who has no referral to them from a Dentist. This includes patients who have already seen a dentist within the practice but there is no referral, the referral does not cover the work being provided by the DCP, or the referral is outside the recall period of the Dentist. The GDC suggests that DCPs consider spending a year post qualification working to prescription in very much the same way as an FD year works for dentists, although this is a recommendation rather than a requirement.
The way dental therapists integrate direct access into practice is very much dependant on the practice set up; until recent changes to NHS guidance and FP17 forms, NHS only practices were not able to benefit from the 2013 direct access mandate. However, with new guidance allowing Dental Therapists and Dental Hygienists to open and close courses of treatment, more practices than ever are looking at taking advantage of a Direct Access model.
Therapists and their practices need to decide between them what services will be offered. It is important to remember that any dental professional can choose to limit their practice to certain treatments, however if working under direct access they must first perform a comprehensive exam and diagnoses within their scope.
When set up with well considered protocols, therapists working within both private and NHS practices will benefit from close working relationships with their referring dentists and a wealth of varied work and support. The practice will in turn benefit from better turnover rates, with dentists being freed up to concentrate on providing private and band three work.
The main current stumbling block for NHS practices is that Dental Therapists cannot prescribe a Prescription only medication (POM) and although this is easily managed in Private practice with a Patient Group Directive document, this is less easy in NHS practices where PGDs would need to be signed by the commissioners: I am yet to hear of this happening successfully. For this reason, NHS Dentists will still need to prescribe Local anaesthetics and Fluoride, which will take some choreographing where NHS practices are hoping to take advantage of Direct Access Dental Therapy.
In a private setting the opportunity for Dental Therapy integration is more flexible and varied than ever before. Therapists can work with their practices to decide what kind of treatments they wish to provide and how this provision will work within the team.
Patients therefore should be encouraged to understand that initial appointments are Dental Examinations and likely only the most routine of treatments could be offered on the day such as cosmetic polishing or general scaling. The General Dental Council encourages all dental professionals to ensure patients have an appropriate amount of time to think about the treatment being offered to them in order to ensure they in full agreement with the treatment plan and this cooling off period is an important step in gaining valid consent.
Deciding on what treatments will be available with the dental therapist will be a very individual process - therapists should take into consideration what treatments they enjoy, are confident and competent to undertake and also regard the practice demographic. For example, Dental practices with a largely family orientated patient base may be inclined to offer paediatric dentistry with the dental therapist as their scope covers much of the treatment required on deciduous dentitions. However dental surgeries should not overlook the value of shared treatment provision, allowing a multidisciplinary approach in practice. General dentists can free up their diary time for more complex restorative work when they have a dental therapist working alongside them providing all the direct restorations required.
Information and Consent
Patients need to be aware of who the clinician is that they are seeing and what that clinician can offer them in terms of treatment and advice. Patients should be well informed prior to their appointment with their Dental therapist. Information they need includes what treatment the therapist will provide on the day, what treatment they can offer following consultation and where they will refer the patient should they need treatment that the therapist cannot provide.
The key to ensuring this works in practice is developing excellent practice protocols and admin workflows.
Areas for practices to consider include:
Will there be a direct access provision or will the therapist work solely under the prescription of a dentist.
Online information -this should be clear details about team members and treatments available including their dental qualifications and any further training they have undertaken.
The information given over the telephone by administrators - excellent training for reception staff which covers the dental therapists scope, what the patient can expect from a consultation and what will happen if the therapist cannot treat the patient
Information sent to patients who book in - this should be detailed and mirror the information on the website and given over the telephone, this information can take the form of a consent form although a physical signature may not always be necessary.
Clear advice from the dental therapist - treatment planning and consultation which stays within the remit set out in the information given in the lead up to the appointment.
Clear knowledge within the rest of the team, especially from dentists who may be treating alongside the dental therapist.
Agreement within the dental surgery of who the therapist will be referring out of scope work to - this could be in house, specifically to dentists with special interests or if required to specialists who do not work in the same practice. The agreement to accept these referrals should be available in writing to avoid confusion.
A written practice protocol ensures that the values of the team and direction that the practice takes when using a dental therapist are consistent and relevant. The protocol should be considered a live document with regular development. This document will outline the overall goal of the team introducing dental therapy, the desired scope of the dental therapist, the information that should be given to patients including how this is delivered and what referrals the dental therapist will make should they be unable to provide all treatment required.
Team working is at the heart of the modern dental surgery and while we watch teams grow and diversify, it is helpful to nurture this growth with supportive and robust written protocols in order to give direction and guidance. Teams who have shared values and a clear direction are typically more likely to be fully engaged and focused on achieving the practice goals together.
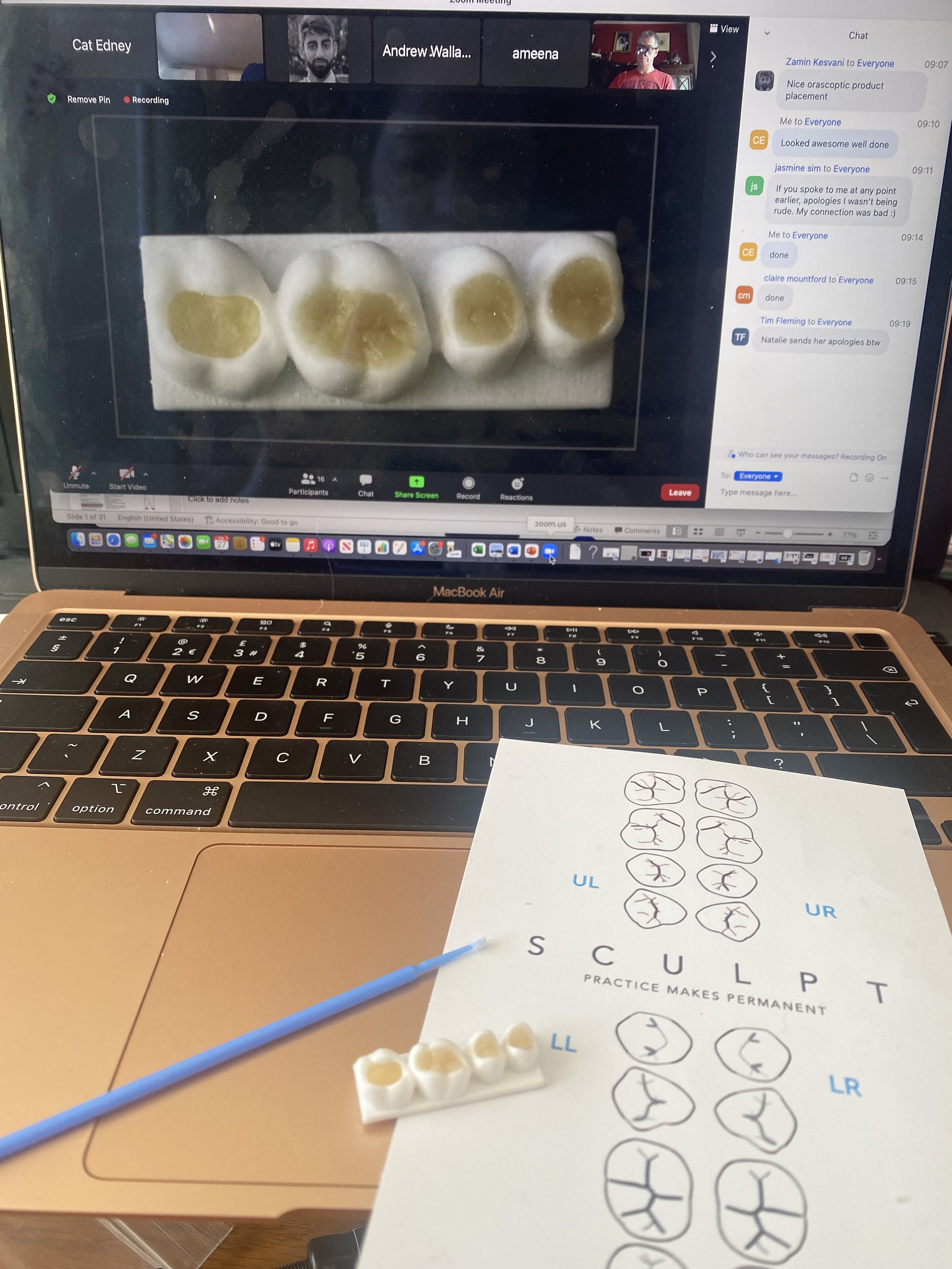
Sculpt - Practice Makes Permanent
Sculpt - a hands on at home experience
Sculpt – a new concept in hands on training
SCULPT started as a yearlong, hands on, online programme designed to simplify morphologically correct composites. Now evolving into an on-demand training platform, with flexible and inclusive learning at its core.
This innovative initiative was the brain child of talented dentist Dr. Shiraz Khan and dental student Curran Patel. Shiraz is hailed for his beautiful composite work and is the aesthetic Dentistry award winner 2021 as well as the director of the young dentist academy.
I was extremely fortunate to meet Dr Shiraz Khan in 2020, I was pre-warned that he was a master of composite and after our meeting I made sure to follow his dentistry on Instagram. To say his work is inspiring is an understatement: so, when he launched SCULPT along with Curran Patel, I jumped at the chance to sign up.
SCULPT is the first, hands-on, online composite course of its kind which means you get a comprehensive interactive experience, guided by true professionals at an incredibly competitive price. As a busy Dental Therapist and mother of three this really appealed to me. Also, the inclusive nature of the course and its marketing means I felt fully encouraged to join as a DCP.
The initial course ran for a year and offered monthly instalments of focused tutorials by Dr. Shiraz Khan. Prior to the course commencing we were sent a full kit of 3D printed, pre-prepped typodont teeth, dental instruments, composite and a light cure.
I was drawn to the idea of learning from the comfort of my own home, without having to take too much time out away from family and I also felt it appealed to my need to develop my skills without the pressure of other people watching me! The flexibility doesn’t stop there with SCULPT now offering an online platform with unlimited access to on demand pre-recorded videos which take you through creating beautifully morphologically correct restorations in a step-by-step fashion.
Also, there is enough kit provided to you to practice the techniques you learn multiple times. The easy-to-follow fissure pattern guide has been invaluable and I have been known to check it mid restoration in practice too.
The instruments are purposefully chosen to be standard style instruments you can find in most dental surgeries - another testament to the inclusive nature of the “SCULPTfam”, ensuring the techniques we learn are easy to replicate in general practice.
In addition to this there is concise and well-chosen pre course material designed to give background to the discussion that takes place on each session; discussing why we use the techniques we do, looking at material choice and bonding protocols to name a few of the topics.
The first session was incremental placement of a class 1 composite on the upper left second molar. Learning more about composite shrinkage, cusp and fissure morphology, correct placement and curing protocols was the added bonus of this session. Dr Khan is passionate about his work and his knowledge is boundless. It was plain to see from the first session that we are being treated to added value just through conversation about the materials and techniques we use.
My first attempt was a little rough and I missed being able to polish up my composite post - placement, however I was pleased with the resulting fissure pattern and to have gained the newfound knowledge of creating supporting cusps and oblique ridge initially and working around these to finalise the restoration.
Working further into the course content we are treated to trying the technique of using a bulk fill composite and carving essential lines to recreate the fissure pattern. This technique had always been a new concept to me and I was excited to learn how we can use it in every day dentistry. Being able to understand the indications and uses of this new technique, and also put it into practice and still build functional and aesthetic restorations was an exciting learning curve. I have felt confident in my composite placement for a number of years but the small tips and tricks that you can pick up from a teacher like Shiraz serve to really enhance your skill and make you proud to show what you can achieve.
The sessions challenge you every time, be it with a new technique, a new instrument or with more restorations to achieve in a smaller amount of time. I have learned to appreciate secondary and tertiary anatomy in a new way and I am no longer needing to polish cusps flatter than I would like them to be!
How can dental practices move beyond the ‘scale and polish’ mindset
No more S&P
Working with a Hygienist or Therapist in practice has become a widely adopted strategy across the UK, however, how that works for each individual can vary widely. It is often reliant on the experience of the hiring practice and team within to be able to understand not only the scope of Hygienists and Therapists but also how to integrate their skills into practice.
There are a number of ways of integrating Hygienists and Therapists into regular treatment modalities within practice, it is important that the practice finds the model that suits them, and the team. Having a great Hygienist or Therapist on board can really build and sustain a business due to the extra patient contact you can work with and the service the patients receive.
The addition of further skills and flexibility around the Hygienist and Therapist scope of practice has seen this role transform into one that can become the supporting foundations of a well-run business. There are, however, still a number of practices who continue to see their Hygienist or Therapist as a ‘tooth cleaner’ – rarely moving beyond scheduling 30minute appointments for 30 minutes of cleaning, reinforcing to the patient the unfortunate message that it is somebody else’s responsibility to keep their teeth clean and healthy.
There are a widely varying number of different ways a hygiene or therapy department can be set up within practice, but the overall ways can be roughly split into four models:
Models:
S&P Only
· Predominantly works with NHS
· Relies on GDP to provide more in-depth treatment and referrals
· Limits treatment success due to time constraints and staff/patient understanding of hygiene treatment
This predominantly out-dated model hails from a time before Hygienists had extended duties and responsibilities.
When considering Periodontal treatment the onus was solely on the dentist to provide complex periodontal treatment and trends in litigation are beginning to demonstrate that often the treatment was limited or seen as secondary to treatment of the hard tissue dentition.
Practices still working to this model are sometimes stuck in a loop of seeing patients with longstanding periodontal inflammation not treated in accordance with the BSP guidelines - often as the Hygiene diaries are full to bursting with short appointments and little scope to expand. Conversely some are empty with a lack of interest in seeing the Hygienist due to lack of support from the rest of the team.
The fix to this issue is to re think the hygienist appointment types, to introduce a periodontal protocol which involves the GDP focusing on educating the patient, and planning comprehensive treatment with the Hygienist. This may mean blocking out sections of the Hygiene diary in order to make space for these sessions. In the long run these patients continue with their regular hygiene maintenance but with healthier, more treatable mouths and longer lasting dentitions.
Full scope Hygiene – GDP referral based
· Gives freedom to follow a protocol for treating perio – better outcomes overall with emphasis on patient education from all team members
· Allows for further treatment planning on Hygienist prescription
· Brings further revenue in the form of fluoride applications, fissure sealants, suture removal and restoration adjustments
· Additional Digital Scanning opportunity can be a cost effective way of promoting patient education and discussing cosmetic treatments
· Hygiene Diary is more flexible and will free up time in GDP diary by removing small treatments from GDP
Most progressive Dental Hygienists are working toward the above model whereby they are able to work to their full scope. The Periodontal treatment planning is carried out by either the Hygienist or the GDP, the Hygienist is also able to maximize their daily profit by providing additional treatment such as fissure sealants or whitening treatments.
The GDP diary has no reflection of a change - but the patients are accessing comprehensive evidence based periodontal treatment and additional treatments are available with the hygienist such as whitening and fissure seals. This reduces surgery time spent on these treatments for the GDP and allows for more free space in the GDP diary for more profitable complex treatment.
Hygienists can also be equipped with digital scanners in order to record patients dentitions, help to monitor soft tissue movements and tooth wear and also promote the conversation around orthodontic work, replacing worn or leaking fillings and to educate patients on their own dental health.
Full scope Therapy –under GDP referral
· As Full scope Hygiene but with additional scope of Therapists
· Frees up GDP diary for Large restorations, Extractions crowns and Dentures
· Can work well in NHS practice if all Band II is referred to Therapist
Often seen more in the North of England, the Therapist is slowly but surely becoming more popular in Primary Care Dental Settings. Traditionally Therapists were only permitted to work in Hospital settings but as legislation changed in 2002 and Therapists were allowed to work to prescription of a Dentist in Practice. The situation improved further when in 2013 Direct Access was approved for Dental Therapists and Dental Hygienists.
By adding the services of a Full Scope Therapist to the Dental practice, you free up time for the GDP to concentrate on the larger and more complex restorative cases. This works especially well with GDPs who have further training in Implant placement, or have a special interest in complex restorative cases. The Therapist is on hand to provide the Class I-V restorations, Whitening, Impressions and Periodontal treatment, they can also be utilised when treatment planning complex cases, taking impressions once the Periodontal condition is stable and generally condensing the GDP diary into check-ups and complex treatments only. The Therapist has time with the patient to reinforce what the Dentist has suggested and talk through any concerns or different questions the patient has. The Therapist may also suggest further cosmetic improvements that have not been covered by the consultation and leave the conversation open for the GDP to pick up.
Therapist Led
• Potential for excellent multidisciplinary approach if more than one Therapist works alongside GDP.
• Treatment coordination and referral time reduced for GDP
Realistically this may need a seismic shift in understanding within the dental Team, but is an entirely possible model when working with a well-trained and integrated team members.
When you move toward a Therapist led model you can start to really see a benefit in multidisciplinary working. If there are multiple Therapists working alongside a GDP, in a close working relationship the Therapist can take over the Routine Check-ups, allowing the GDP more time for case planning and high profit treatments. With more than one Therapist working alongside a GDP the diaries can be arranged for the GDP to oversee treatment plans and pop in to the Therapist check-ups in order to review and agree any complex treatment required. The model requires exceptional team working and communication but ultimately reduces lone working and gives patients a phenomenally eefficient service.
This model works best under the Direct Access arrangement.
· Can be a good additional stream of revenue for Hygienist / Therapist Diary
· Excellent practice building potential
There is also a softer way of integrating the Therapist led model, by means of GDP initial consultations for new patients, and Therapists undertaking the routine examinations thereafter. The GDP is still referred to for complex treatment planning, and makes themselves very visible during the Therapist appointment in order to maintain the relationship with the patient and demonstrate a well-integrated and approachable team.
There is a ingrained sense of uncertainty in some Dental Surgeries around utilising their Hygienists full skill set or the Therapists full scope. Often because the diary management hasn’t changed for many years or the previous person in that role was not trained in additional skills later added to the Scope of Practice. Practices ought to take the lead from their Hygienists and Therapists, exploring together the ideal set up and ways to make that happen. The additional revenue, patient contact and patient care can be an invaluable addition to a successful business, and a happy team.
Why I bought my first set of loupes in 2021 even though my eye sight is still 20:20
Seeing clearer for 2021
Before my cohort qualified in 2008 one of the first trades to contact us was loupes companies offering us student discounts and free measuring and fitting services. As many of my colleagues duly bought their loupes - I was hesitant and resisted spending the cash. This was in most part due to finances but also having had no experience of using loupes I wasn’t sure what I was missing - or even that there was anything to miss.
Many of the dentists I was working with at the time were not using loupes and so I felt as a therapist I probably didn’t need them either. Fast forward to 2021 and although my vision is 20:20 still I’ve noticed a surge in the number of my colleagues who use them. It has been getting to the stage in my practices where not using loupes for restorative cases was becoming unusual. Loupes had also been at the front of my mind during the 2020 pandemic while I was fit testing hundreds of dentists and dental care professionals who needed to ensure their FFP3 and P3 respirators would fit alongside their loupes. It was at that stage that I decided it was time for me to look again at getting a pair.
Many of my colleagues have had to forego using their loupes while wearing FFP3 respirators due to the difficulty of getting a good fit while also keeping their correct working distance and angulation. I was concerned that I would be investing in kit that may be redundant for some time so I reached out to Joe at Q-optics and discussed my concerns. Joe explained to me that they would be able to give me a range to try, give me time to check my chosen style and size works with my current respirator and offer a lifetime support and guarantee.
I was pleasantly surprised by the ease of ordering, Lorraine from Q-optics arrived at my practice with a large case brimming with options. The case was layer upon layer of frame styles, colours, sizes and magnification options. She patiently allowed me to test each style, I was able to try my respirator options and had plenty of time to fit check each one. I chose a style that fitted me comfortably and felt compatible with my current PPE and personal surgery set up. It was very helpful to have Lorraine come to my surgery so I could sit in my own chair for measurements - she was extremely thorough making sure that my posture and working distance were correct. We discussed light options and I was able to try a wired and wireless version to feel the difference and get more of an understanding of what option would work better for me.
Q-optics also developed their own visors which helpfully clip on to the frame of the loupes and have a cut out so that my light isn’t reflecting back at me, the case they came in was personalised and is compact enough to easily fit into my camera bag. These touches make all the difference when ordering especially as a Therapist I move between surgeries and practices and I need my equipment to be well protected at all times.
Since working with Loupes; I have become converted along with so many people who say they can’t believe they worked without for so long! I feel like my posture is better - my chiropractor is missing my regular visits. Additionally, my patients seem to sit better, almost as if they are taking the appointment more seriously because of the kit I am using. I have really seen the benefit of having that illuminated magnification and although it has taken some getting used to, the loupes no longer feel difficult to get into the right spot.
What frames should I buy?
I would say try all of the frames to find something that you are comfortable in. Try them with both an FRSM and your FFP3 to ensure that they fit well on both and do not compromise the seal of your respirator. I went for square frames because as a non-glasses wearer I have always wanted a set of square frames however helpfully these also fit me and all my mask options well! I would say if you are used to Hogies style wraparound safety glasses the options from Q-optics are very comprehensive and you can choose from lots of colours!
What Light should I get?
This question is very important, you should consider how long you will be using your loupes for each day and also how easy is it for you to charge your light.
For me, I work part time and don’t use the loupes for hygiene maintenance appointments so I decided on a wireless light.
If you are wearing the loupes all day a wired light is likely to have longer battery life and see you through the day.
Charging both lights is really easy and my wireless light came with two batteries which just clip on in seconds.
How can I ensure they fit me?
Trust the rep that comes to you and try lots of styles. Try to make sure that when your working length is measured you are really sitting in your ideal position and ensure that you try the loupes with a light attached so that you can feel the weight of them.
How long does it take to get used to using them?
It really only took me one or two patients of use to feel entirely comfortable however I did spend some time with them at home making sure that I was able to adjust the light position and get them on and off again easily. It is normal for people to feel a little dizzy the first few times they wear them or to get a small headache. In these situations; try wearing for one or two patients a day and build up to wearing them more.
What happens if they break?
Q-optics give a lifetime warrantee on their loupes which is what really attracted me to them - I have three small children and I move between surgeries and practices daily so I needed to know I would be supported if my loupes needed a little TLC.
What kind of maintenance is involved?
The case came with special cleaning fluid and cloth to keep the lenses clear and clean. Other than that all you need to do is charge your light battery. They really feel robust even though they are very light and as a busy clinician I am pleased that there is very little needed to keep my loupes in good condition!
Special Care Dentistry – How Dental Therapists are contributing to caring for the neurodiverse and those with special needs.
It all begins with an idea.
Cat Edney talks to two Special Care Dental Therapists about their role
Very occasionally, a job of the rarest variety is posted on NHS jobs; Special Care Dental Therapist.
These roles are rare but also highly regarded in the Dental Therapy world as incredibly rewarding. My own experience of working in special care was limited to a precious few months during my training at Kings College London, some Therapists however have taken this role and have flourished. With Dental Therapy becoming increasingly utilised in general practice, I wanted to find out more about how the Therapist role is used within the Special Care Team and how Dental Therapy can help to manage the demand for this service within the NHS.
Andrea Powell is in community Special Care in Wales, Vikki Griffiths works in the Liverpool Dental Hospital
Can you tell me more about your work?
VG
I work predominantly as a Dental Hygienist / Therapist on a Special Care Department at Liverpool Dental Hospital. I work alongside special care Consultants and specialty Dentists, registrars and dental students.
I am the only Dental Therapist on special care, and all of the above refer patients to me for a range of dental treatments.
Working on special Care is really different to seeing patient’s in general dental practice – I have to do a lot of pre-treatment planning before my patients arrive. I have to check any correspondence from referring dentists, previous treatment history. Some patients with learning disabilities have triggers which I need to know about before they come into the surgery. I also review blood reports (if required), radiographs and if the patient has any additional needs such as the use of a hoist, Saturn turner, bariatric trolley or Ambulance transport. Some of the patients I see require extra time and attention and I am lucky I have that on my side – each appointment with me is a minimum one hour long – I extend this if required again dependent on the patients’ needs and requirements. I also have a Patient Group Direction set up so this helps appointments run smoothly and allows me a little freedom when treating my patients.
AP
In community I see children from low socio-economic groups and ethnic minority areas. Some of these children are in the “at risk” category most of them have a high caries rate due to poor diet/oral hygiene education at home.
Some of the patients I see are adults with additional needs, such as Down’s Syndrome, Global development delay, patients who are peg fed and other forms of neuro diversity.
What kinds of patients do you see?
VG
Each day is different on Special Care! – I see a wide variety of patients from young to elderly adults. The patients I treat usually have very complex medical histories – so it’s really important for me to liaise with my senior colleagues, especially at the moment as I am new to working in special care.
I treat patients with learning disabilities this can range from mild to severe, blood disorders such as hemophilia or von Willebrands, Patients with cancer – this varies from blood cancer (myeloma, leukemia or lymphoma) other cancers of the body or head and neck cancers. I also see patients who have very complex medical histories. This list is endless!
Did you do any further training to be able to treat special care patients?
VG
I didn’t have any additional training other than my Diploma in Dental Hygiene and Therapy when I started at the hospital. However, I did have over 10 years hospital experience as a specialist Dental Nurse – this could have been a factor why I was successful with my application?! Who knows!
I am currently looking into courses to help build my knowledge and skills base. I looked into a special care course but, the Diploma in special care dentistry is currently only open to Dentists – which is disappointing and I’m hoping this changes or another course directed at Hygienists/Therapists is developed. Inhalation sedation is something I would like to provide to a selection of my patients, so this is a course I’m keen to complete soon.
AP
I didn’t have any further training.
What sorts of treatment do you normally provide?
VG
I use my full scope of practice when treating patients on Special care, although Hygiene treatment forms the basis of the referrals I receive, each patient usually needs restorations, impressions, and radiographs in addition to this.
Sometimes my treatment is simply just acclimatizing a patient and carrying out Oral Hygiene and building appointments up from this to the more complex treatments.
AP
The treatment I provide ranges from oral health education and acclimatisation to full mouth restorations due to caries, referring anything not in my scope of practice to other dental colleagues.
Do you feel these patients could be seen in general practice?
VG
During the time I have worked on special care there has probably been one or two patients who I felt could have been seen in general practice.
All of the patients seen on SCD at Liverpool are referred in by their GDP and each referral is accessed by the consultant to ensure their suitability. Sometimes patients come in with an unstable condition and then it stabilises throughout the treatment plan. Each patient is usually accessed and once treatment plans are completed if suitable they are referred back to their GDP. This is to ensure the service is accessible to the patients who require it.
AP
I do believe that some of these patients could be seen in general practice along with their family members. The main reason for seeing them in a community setting is time. There are no financial elements when working in the community which allows time to be used more freely.
What are your top tips for managing special care patients?
VG
· Never underestimate the effect a smile can have on a patient.
· Have patience and understanding for your patients.
· Sit and Listen to your patient.
· Never assume!
· Your Dental Nurse is invaluable when treating special care patients – they have magic powers!!
AP
My top tips for seeing patients with neurodiversity and special needs in general practice would be continuity and patience. Neurodiversity and special needs are, as we know, a spectrum so one label does not fit all individuals. What works well for one patient can vary hugely to the next. I feel that you can get a feel for how things will go on a first visit. Try, where possible to have the same DCP from start to finish to build a rapport with your patient, much the same was as we do on a day-to-day basis with all patients. Give your time and understanding without limits.
Don’t clock watch, give yourself long appointments, it is better to have too much time that is not needed than too short a time and feel rushed, this will be picked up by the patients and can hamper your best efforts.
How do you feel about your job?
VG
I love my job! As cliché as it sounds I feel I am in my dream job. Although it isn’t always sunshine and rainbows I enjoy the diversity and the challenge I feel as a clinician. I have learned so much in the last 8 months and I don’t feel I have even scratched the surface yet! No two days are the same on Special Care …. ever!
AP
I love working with patients with extra needs as I know that I am giving them care where in general practice they may not have the surgery space or time as we all know, the pandemic has greatly increased our appointment lengths so waiting lists are longer.
I get an enormous sense of well being doing my job. My job satisfaction is right up there. I enjoy going to work, knowing that I am going to see some of my favourite patients who are genuinely pleased to see me too.
How can the dental community better serve patients with special needs or neurodiversity?
VG
From what I’ve experienced, Dental community dental services do a brilliant job of treating patients with special or additional needs and adapting to their needs.
I think there should be an option for patients to see CDS on a regular basis not just a ‘treatment only’ basis as I feel the patients would benefit from regular continuity of care, especially as the clinicians who work in community are so skilled.
AP
Many dentists have all said that they would be happy to see patients in practice if the individual with extra needs was tolerant of dental care, but feel that any person whose needs are more complex would be referred to the community setting as they know that time is not an issue.
Some parents feel that they would like their child to be seen with the family dentist where possible so as not to single out the child for their differences/extra needs. However, on the flip side, some parents feel that their child will be better looked after in a community setting.
There are no right or wrong answers here and a conversation needs to be had with the care giver, patient (where possible) and DCP to place the patient in the best dental setting for each individual.